Canberra parathyroid surgeon
The Patient Journey

1
Immediate pre-operative ultrasound to locate parathyroid adenoma

2
Planned surgical approach
3
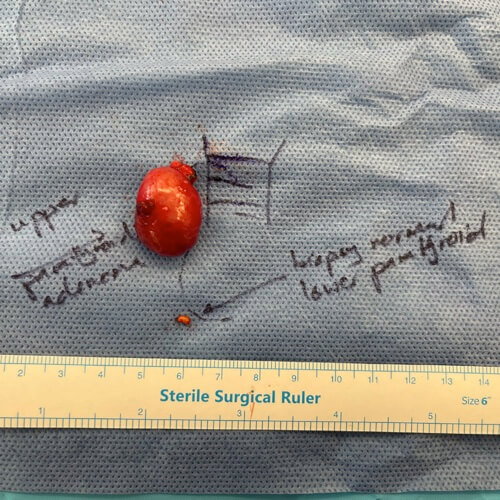
Post surgery image of removed parathyroid adenoma

4
Post surgery image of removed parathyroid adenoma
What Type of Operation is Best to Treat Hyperparathyroidism?
This is a topic of some debate in the contemporary endocrine surgical world. The answer is that a universal approach cannot be applied to every person.
Some observation summary points regarding the different approaches are made below. It is important to emphasise that every person with a diagnosis of hyperparathyroidism should have their unique situation and circumstances assessed and discussed with their expert Endocrine Surgeon.
Unilateral / Focussed or minimally Invasive Parathyroid Exploration
- With an experienced endocrine surgeon, good imaging / X-ray localisation and good operative tools the long term cure rate is around 95-98%
- Shorter operation time – typically around 30 minutes
- Complication rate for minimally invasive surgery is very low
- Smaller wounds and quicker recovery.
Typical Patient Journey Images for Unilateral or Minimally Invasive neck Exploration for Parathyroid Adenoma

Ultrasound used to localise known parathyroid adenoma position immediately before Surgery. Skin incision planned and placed in adjacent skin crease (for long term best wound healing and invisible scar)
Pre-operative:
Calcium 2.82 PTH 15.1
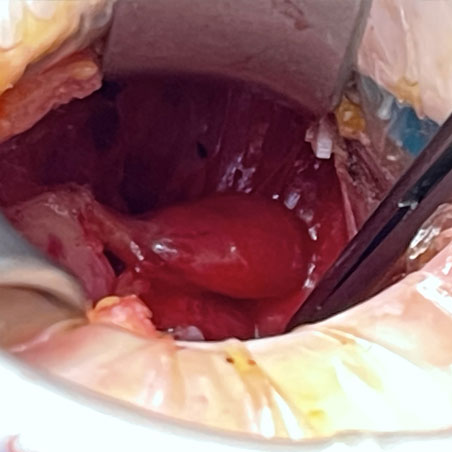
In minimally invasive surgery, parathyroid adenomas can be removed in a brief and targeted procedure.
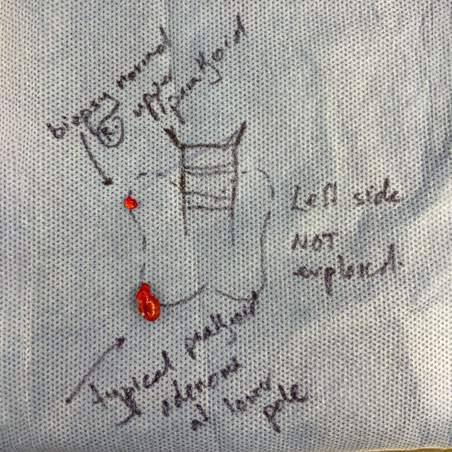
Moderate sized but typical parathyroid adenoma at right lower gland position removed. Small normal right upper parathyroid gland biopsied for confirmation.
Post-operative:
Calcium 2.17 PTH 3.9
Full Bilateral Neck Exploration or 4–Gland Exploration
- In experienced endocrine surgeon hands a 98-99% long term cure rate
- Larger wound and longer operative time
- A slightly higher complication rate including a small rate (between 1-10%) of hypocalcaemia (low blood calcium requiring supplements) post-operation
- Bilateral 4-gland exploration is the appropriate operation in the circumstance of hereditary hyperparathyroidism or M.E.N. Syndrome (multiple endocrine neoplasia).
Complications of Parathyroid Surgery
Whilst long term, serious complications of parathyroid surgery are rare it is important to be aware of the possibilities.
Common Complaints or Problems after Parathyroid Surgery:
- Some swelling or stiffness around surgical wound – this is common and virtually always resolves spontaneously over 2-3 weeks. Physiotherapy / massage is a good remedy.
- Stiff neck that requires some physiotherapy afterwards
- Very minor / subtle changes in voice are reasonably common – but usually very short lived, normally resolving within 1-2 weeks of surgery.
Rare Problems After Parathyroid Surgery: ( around a 1-2% chance )
- Wound infection – genuine wound infections after neck surgery are known to be very rare.
- Long term or serious change in voice quality
- Persistence or recurrence of the high calcium can occur relating to not finding all abnormal parathyroid glands
- Bleeding or bruising in the tissue that requires some form of intervention to remedy it
Thyroid and Parathyroid surgery is a field that has benefited greatly from the development of sophisticated technical tools.
The very design and execution of your parathyroid operation is carried out with the aid of these special technical tools in order to minimise the chance of serious problems:
- To minimise bleeding risks an Ultrasonic shear is used to coagulate small blood vessels. Fibrin glue products are also available and regularly used to prevent bleeding complications.
- Magnification is used to aid in identification of important small structures in the neck particularly around the parathyroid gland
- Sophisticated electrical neuro-monitoring techniques are used to ensure the integrity of the important nerves that mediate voice and singing
REFERENCES
Delbridge L. How to Treat: Primary Hyperparathyroidism. Australian Doctor. July 2019 p15-19.
Learn more about A/Prof A-J Collins at his website
For Canberra consultations, phone
(02) 6282 1191
For Bega consultations, phone
(02) 6491 9559
For any other enquiries, email
reception.ajcollins@gmail.com
For any other enquiries,
Email us
©2022- A-J Collins PRIVACY POLICY DISCLAIMER Website by: